With excellent healthcare infrastructure, a skilled and multilingual workforce, and a richly diverse population, Australia is an appealing destination for conducting clinical trials. Each year, this nation hosts thousands of new clinical trials, from first-in-human (phase 1) to post-market (phase 4), spanning a range of therapeutic areas. In fact, Australia has such a highly active trials community that from 2006 to 2020, over 18,000 trials with recruited participants were registered. This number is only increasing, with 40% of those trials occurring in the period between 2016 and 2020.
Australia is also an appealing destination due to the rapid nature of study start-ups, and understanding the ethical and regulatory requirements and processes is key. So, how can sponsors and researchers expertly navigate the Australian clinical research start-up activities to conduct safe, compliant, and scientifically sound clinical trials in the shortest possible time?
To answer these critical questions, we’ve put together this best-practice guide to conducting clinical trials in Australia. Whether you're a seasoned researcher or new to the field, it will equip you with the knowledge needed to thrive in the Australian clinical research space.
There are multiple advantages that make Australia a prime choice for clinical studies. From accelerated trial initiation to a streamlined regulatory process to generous government funding, here are six reasons why you should consider conducting your clinical trial in Australia.
One of the most compelling reasons to choose Australia is the speed at which you can get your study up and running. Australia's efficient start-up procedures include streamlined approval processes and standard templates for agreements, which means your clinical trial can commence faster than in many other countries. In fact, studies can commence in 8 weeks at private sites, which is many months faster than in the US. This acceleration saves you time and resources, a crucial factor in product development and medical research.
In the pursuit of groundbreaking medical discoveries, financial support is paramount. The Australian Government understands the value of medical research and has made significant investments to support advancements in healthcare and entice researchers to come to and stay in the country. It offers a generous Research and Development (R&D) tax offset, which includes a potential 43.5% Government rebate on clinical trial spend for companies. By choosing Australia for your clinical trials, you can tap into these substantial financial incentives and reduce your overall costs.
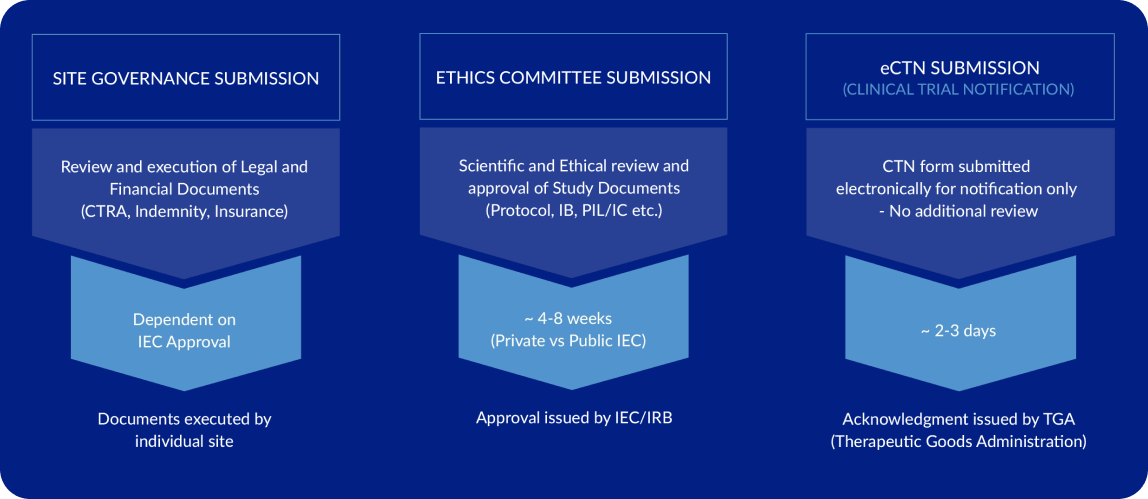
Australia boasts a regulatory environment that is both robust and transparent. Its ability to maintain rigorous standards while expediting the regulatory process sets the country apart. An Investigational New Drug (FDA IND) style application is not required in Australia for most interventions. Rather, the ethics and scientific committees connected to the study sites review the document packages and make the decision to conduct a trial. While the ethics committee is reviewing the package, the contract and budget documents can be submitted concurrently to the site-specific Governance Office. As the legal language of the contract is standard across Australia, the focus here is on budget negotiation. Meanwhile, the Clinical Trial Notification (CTN) can also be submitted to the TGA. This electronic process takes just 2-3 days on average as there is no documentation review. A single site can be included in the initial notification to TGA, and additional sites can be easily added as they come online for a small fee.
Australia's healthcare infrastructure is world-class, providing the perfect ecosystem for clinical research. A 2021 analysis of 11 high-income countries’ healthcare systems saw Australia ranked in the top three, alongside Norway and the Netherlands. In particular, Australia was recognized for its healthcare outcomes (#1), equity of care (#1) and administrative efficiency (#2). An efficient healthcare system, top-tier medical facilities, and advanced technology ensure that trials can be carried out with the highest standards of care and precision.
Now, let’s delve deeper into the specifics of how Australia maintains these high standards. We’ll explore why the country's approach to clinical trials is not about taking shortcuts but abiding by a regulatory system that works for researchers and patients.
Australia has a culturally and ethnically diverse population, which makes it an ideal location for clinical trials. The country has one of the world's oldest continuous cultures and a population that represents over 300 ethnic backgrounds. Australia is also home to widely-distributed age demographics, with the highest representation in the 30-39 years bracket.
By conducting your clinical trial in Australia, you’ll have access to a wide range of ethnicities, genetic backgrounds, and age groups in order to enhance the universal efficacy of your trial results. This diversity can be a game-changer for drugs and treatments intended for a global market.
Australia prides itself on its highly skilled and dedicated healthcare workforce. From clinicians and investigators to industry research professionals, Australia is home to a pool of experts who can contribute to the success of your study. The government is committed to maintaining this workforce, with a 10-year National Medical Workforce Strategy in place to ensure that the country can meet the ongoing health needs of its population. One of the primary focuses of the strategy is guaranteeing a balance of health workers across different specialties and geographic locations. To support this regional strategy, Southern Star Research also has experienced staff members located around Australia.
At the core of Australia's clinical research regulatory framework is the Therapeutic Goods Administration (TGA). The TGA is Australia's equivalent of the FDA in the United States, responsible for overseeing and regulating the quality, safety, and efficacy of therapeutic goods, including pharmaceuticals and medical devices. It plays a pivotal role in ensuring that clinical trials are conducted according to the highest standards.
The TGA provides comprehensive guidelines and requirements for conducting clinical research in Australia. Sponsors and organizations embarking on clinical trials must meet these expectations, as outlined in the clinical practice handbook.
The Australian Clinical Trials Handbook published by the TGA, offers valuable insights into the legal aspects of running clinical trials in Australia. It covers essential details of the Australian regulatory environment, including manufacturing and import requirements for both drugs and devices. Before you start your clinical trial, it is worth familiarising yourself with this handbook and discussing key items in your program with an experienced and well-versed CRO.
Human Research Ethics Committees (HRECs) are another critical aspect of the Australian clinical research landscape/environment. These committees are responsible for reviewing and approving research protocols to ensure that trials are scientifically sound and conducted ethically in the participants' best interests. Key ethical considerations such as informed consent, participant protection and risk minimization are central to HREC evaluations.
There are around 200 HRECs across Australia. While the HRECs operate independently and are often associated with universities, hospitals or research institutions, there are opportunities for mutual recognition of review. There are also private HRECs that review applications of private facilities. The National Health and Medical Research Council (NHMRC) provides a list of accredited HRECs.
The current version of the manufacturing company’s Investigator's Brochure (IB) is required. This should be in the format outlined in the International Council for Harmonisation (ICH) Good Clinical Practice (GCP) Guidelines and include all information on the development of the intervention to date.
This Sponsor-approved protocol reflects elements documented in ICH GCP Appendix B. The protocol is the global standard document that stipulates activities required to collect the defined dataset and how your trial will minimize and mitigate risk to ensure the wellbeing of participants and trial integrity.
Informed consent is a cornerstone of ethical clinical research and the documentation and process used to consent trial participants must be submitted to the HREC. HRECs rigorously assess the profile of participants, the materials provided to them, and informed consent processes to safeguard the rights and well-being of trial participants.
All documents that will be provided to participants are to be submitted, including questionnaires, advertisements, participant information cards, letters of invitation, diaries, interview questions, telephone scripts and so forth. Any materials provided electronically during the trial must be presented as closely as possible to how they appear on each screen of different types of devices.
The Clinical Trial Notification (CTN) scheme is the most frequently used pathway and streamlines trial start-up. As the name suggests, the CTN is a notification to the TGA and permits the supply of unregistered therapeutic goods through a clinical trial. The CTN is submitted electronically and details the key stakeholders in the trial and all unapproved products supplied. Once the CTN is acknowledged and the HREC and governance approvals are in place, the clinical trial can commence in Australia.
The Clinical Trial Approval pathway is more like the FDA IND pathway and is mostly used for Class 4 biologicals, that is, high-risk biologicals, including products with live cells, stem cells or derived from stem cells, derived from human cells.

Site management and monitoring are the engines that drive the day-to-day progress of your trial during the active data collection phase. The Clinical Operations team members work closely with trial sites to ensure timely coordination of activities and oversight of data and processes. Together these contribute to protocol adherence, clean data and effective working with sites to ensure the safety of participants.
Safety monitoring and reporting in Australian clinical trials involve continuous tracking of adverse events (AEs), immediate reporting of serious adverse events (SAEs) to regulatory bodies and ethics committees, and meticulous documentation by investigators. Trial sponsors oversee the safety monitoring process, ensuring compliance with NHMRC guidelines and reporting to the TGA. Human Research Ethics Committees (HRECs) review safety reports to ensure participant welfare, while Data Safety Monitoring Boards (DSMBs) may periodically review safety data to recommend trial modifications. This framework, aligned with international standards, ensures comprehensive safety management and reporting, safeguarding participants and research integrity.
Ensuring compliance and maintaining the highest standards of quality is non-negotiable when conducting clinical trials globally, and there are no exceptions in Australia. This chapter explores the essential components underpinning this commitment, focusing on the Good Clinical Practice (GCP) guidelines and National Statement that guide successful clinical trial conduct in Australia.
ICH is the bedrock upon which ethical clinical trials are built and provides a framework for the design, conduct, performance, monitoring, auditing, recording, analysis, and reporting of clinical trials. In Australia, compliance with ICH Good Clinical Practice (GCP) guidelines is required. You also need to consider the National Statement on Ethical Conduct in Human Research, published by the National Health and Medical Research Council (NHMRC). Adherence to local and global guidelines is a fundamental requirement and ensures the reliability and credibility of your research outcomes.
The ICH GCP guidelines emphasize key principles such as:
Quality control is the systematic approach to ensuring that clinical trials consistently meet established standards. It encompasses processes, procedures, and checks that validate the accuracy, completeness, and reliability of trial data. Quality control measures include ongoing training for staff, consistent documentation practices, and maintenance of standard operating procedures (SOPs). Maintaining a robust Quality Management System is integral to the success of your clinical trial. A good Clinical Research Organization (CRO) can fully integrate this for you, ensuring the highest standards of participant safety and data integrity throughout the study.
Regular monitoring and auditing help identify any deviations from the regulations, guidelines, procedures and study-specific documents, including protocol. Continuous reviews also allow timely corrections and improvements throughout your clinical study and support the trial sites in their activities. The goals of monitoring are to ensure participant safety and data integrity. Auditing aims to assure the integrity of your data and the wider research process, enhance trial quality, and provide sponsors and regulatory authorities with the confidence that your trial is conducted reliably and ethically.
Data integrity is a cornerstone of clinical research. Ensuring that your data is complete, accurate, and reliable is essential for the validity of trial results. Your practices to ensure data integrity should encompass data collection, management, and analysis focusing on preventing data breaches, inconsistencies, or errors. Monitoring by Clinical Research Associates (CRAs) and Data Management (DM) staff is key to data integrity. Only the CRA gets to see the medical records of each participant and can confirm the Electronic Data Capture system (EDC) accurately reflects trial events and participant data. Robust systems and rigorous data integrity safeguard the credibility of your clinical trial findings and ensure the value of your work.
The nuances of quality and compliance in clinical trials emphasize the significance of maintaining rigorous standards and documentation. The guidance of a CRO can be instrumental to this, providing the expertise and experience needed to meet these critical objectives and ensure that your clinical trial stands as a paragon of ethical and scientific excellence.
Clinical research has no guaranteed certainty, so it's not uncommon to encounter challenges along the way, regardless of where you conduct your trial. So, here’s some guidance on how to navigate these challenges, ensuring that your clinical trial can progress without significant drawbacks.
Australia is a vast country, and conducting trials in remote or rural areas can be logistically and operationally challenging. Rapid development in electronic systems including personal devices have facilitated mechanisms for more of our population to be included in clinical trials. Accessibility, infrastructure, and patient recruitment may still present issues; that’s why it’s important to consider the following:
Bonus tip: Keep an eye out for financial support! The Australian State Government has previously offered grants to eligible organizations conducting clinical trials in rural, regional and remote areas of Australia.
The complex supply chain and logistics of clinical trials require careful management to avoid delays and disruptions to your study. Here’s what you can do:
Collaborating with team members, investigators, and stakeholders in different time zones can present scheduling and coordination challenges. That’s why it’s important to ensure the following measures:
With the right knowledge and processes to adhere to the highest ethical standards and regulatory requirements, you can conduct your clinical trial in Australia with confidence. Throughout your clinical research journey, the support and localized knowledge of a Contract Research Organization (CRO) can be your most valuable asset. Your collaboration with a CRO is a partnership in problem-solving, ensuring that your clinical trials progress with efficiency, quality, and scientific merit, ultimately contributing to your research success and the advancement of healthcare worldwide.
L1, 1 Merriwa Street,
Gordon, NSW, 2072 Australia
Connect with us
Keep up to date with the latest news, updates and promotions
Each member of our Leadership Team boasts an average of 30 years experience. Our clients have access to an extraordinary group of Clinical Research professionals, whose experience covers Multinational Pharmaceutical companies, Biotechnology, Medical Device, CRO’s, research institutes, Universities, Industry Associations & Government Bodies. Together, we ensure that every aspect of your unique and novel drug study clinical trial is handled with scientific precision, care, and foresight.
Our team has all of the tools, knowledge and experience to solve almost any issue that may arise during the complex clinical trial process.
We recognize that each study is unique and different and there are nuances that need to be resolved proactively.
Our advisory board of top-tier specialists in multiple therapeutic areas engage in the early stages from protocol design in constructive discussions to anticipate challenges and enhance study efficiency throughout the study.